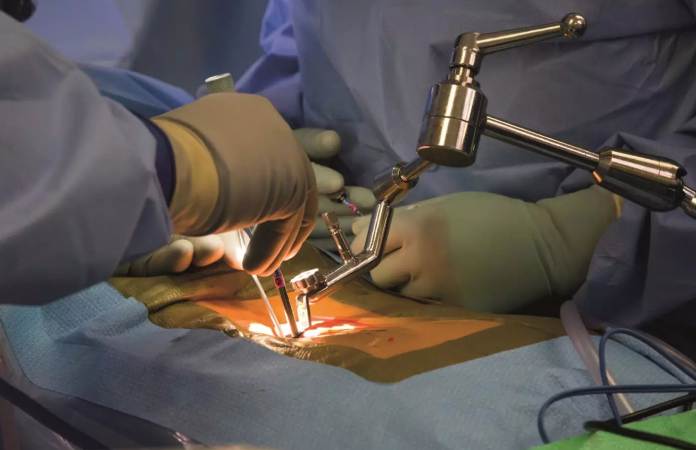
Minimally Invasive Spine surgery (MIS) has dramatically changed the recovery process for athletes with spinal injuries, providing a faster and less disruptive option than traditional open surgery. The use of smaller incisions, advanced imaging technologies and specialized surgical tools allows for less trauma to surrounding tissues, enabling athletes to recover more quickly. Dr. Larry Davidson, a highly regarded specialist in minimally invasive spinal surgery, has helped pave the way for these innovative techniques, which have been particularly beneficial for athletes seeking a rapid return to competition. However, despite the advantages of MIS, the role of physical therapy in optimizing recovery cannot be overstated.
Physical therapy plays a pivotal role in enhancing recovery after minimally invasive spine surgery. It focuses on a tailored approach that integrates strength-building, balance training and sport-specific exercises. These personalized rehabilitation strategies ensure that athletes recover safely and regain their full functional capacity, allowing for a smoother and faster return to their sport.
Early Movement: The Key to a Speedy Recovery
One of the first milestones in recovery after minimally invasive spine surgery is early movement, which helps maintain flexibility, improve circulation and prevent stiffness. Unlike traditional open surgery, which typically requires extended bed rest, early mobilization after MIS is essential for preventing muscle atrophy and maintaining muscle tone. Physical therapists often guide athletes through gentle movements starting within a few days of surgery to help reduce swelling, promote blood flow and enhance the healing process.
Functional Benefits:
- Preventing Muscle Weakness: Early movement helps prevent the rapid loss of muscle mass that can occur with prolonged immobility. It also ensures that the muscles supporting the spine remain active and engaged.
- Improved Circulation: Mobilization helps reduce the risk of blood clots by promoting better circulation, while also delivering nutrients to healing tissues, accelerating recovery.
Athletes who begin movement early are generally able to return to physical activity much quicker than those who delay rehabilitation. The sooner they begin engaging with physical therapy, the sooner they can start strengthening their muscles and restoring their mobility.
Strength-Building and Core Activation
As the healing process progresses, strengthening the core muscles becomes a critical part of the rehabilitation process. Athletes rely on a strong core for stability, posture, and movement control. After spinal surgery, these muscles often weaken, making it more difficult to maintain proper posture and spinal alignment. Targeted rehabilitation exercises, such as bridges, pelvic tilts and planks, help to restore core strength and stabilize the spine.
Core Rehabilitation:
- Basic Movements: Early core exercises focus on engaging the deep stabilizing muscles, without overloading the spine. These movements include pelvic tilts and bridges, which help to activate the lower back and abdominal muscles.
- Progressive Strengthening: As recovery advances, more challenging exercises like planks and leg raises help improve overall core strength, which is vital for spinal support and athletic performance.
Building a strong core not only supports the spine but also improves posture, flexibility and balance, all of which are crucial for athletic performance. Core stability exercises allow athletes to perform daily activities with more confidence. They also play an integral role in preventing future injuries, by ensuring that the spine is well-supported during physical activities.
The Role of Balance and Coordination
In addition to strength-building, balance and coordination exercises are essential for athletes recovering from MIS. After surgery, athletes may experience altered movement patterns as they try to protect the surgical site. Dr. Larry Davidson explains that it can lead to compensatory movements that place additional stress on other parts of the body, potentially causing new injuries. Proprioception training, which focuses on improving body awareness and balance, is a key part of rehabilitation.
Balance and Coordination Training:
- Proprioception Exercises: Standing on one leg, performing balance drills or using unstable surfaces like balance boards helps athletes rebuild their body awareness and stability.
- Dynamic Drills: More complex movements, such as lateral stepping drills or agility exercises, are gradually introduced to help restore functional movement patterns that mirror the athlete’s sport.
By engaging in balance and coordination exercises, athletes can improve their body awareness, reduce compensatory movements and ultimately reduce their risk of injury when they return to sport. These exercises ensure that athletes regain control of their movement and confidence in their body’s abilities.
Functional Rehabilitation: Returning to Sport
After regaining strength, flexibility and balance, athletes enter the functional rehabilitation phase. This phase focuses on simulating sport-specific movements and building endurance and coordination. For athletes recovering from minimally invasive spine surgery, rehabilitation should gradually progress to more intense exercises that mirror the physical demands of their sport.
Sport-Specific Exercises:
- For Runners: Agility drills, interval sprints and endurance running exercises help athletes regain cardiovascular endurance and leg strength, while minimizing spinal stress.
- For Swimmers: Swimming-specific drills are introduced, focusing on shoulder stability and core strength.
- For Cyclists: Cycling training on stationary bikes or through controlled outdoor rides helps rebuild leg strength and cardiovascular capacity.
By progressing through sport-specific exercises, physical therapy ensures that athletes are prepared for the unique demands of their sport. It allows them to safely return to competition, while minimizing the risk of re-injury.
A Holistic Approach to Recovery
The success of recovery after minimally invasive spine surgery relies heavily on a structured rehabilitation plan that goes beyond the surgery itself. While MIS provides athletes with a faster recovery time and less disruption to surrounding tissues, the path to full recovery requires careful management. It includes not only restoring physical strength and mobility but also addressing the psychological aspects of rehabilitation. The mental hurdles that athletes face are just as crucial to recovery as the physical aspects.
Recovery after minimally invasive spine surgery involves a well-rounded, holistic approach that addresses both the physical and mental aspects of recovery. Successful recovery hinges on a well-designed plan that incorporates early movement, targeted physical therapy and gradual reintroduction to sport. This multi-faceted approach ensures that athletes not only heal but also become stronger and more resilient, reducing the likelihood of re-injury when returning to high-level competition.
Maximizing Recovery through Physical Therapy
The role of physical therapy in optimizing recovery after MIS cannot be overstated. While MIS provides the foundation for a quick recovery, early movement, core strengthening and functional rehabilitation are essential to ensuring long-term success. By engaging in a carefully structured rehabilitation plan, athletes can not only recover but also return to their sport stronger, more resilient and better prepared to handle the physical demands of competition.
True rehabilitation goes beyond healing; it prepares athletes to step back into their sport with renewed strength and resilience. By pairing early mobility with personalized training, athletes regain confidence, protect against re-injury and set themselves up for long-term success.